Mayer-Rotkitansky-Kuster-Hauser Syndrome
Mayer-Rokitansky-Kuster-Hauser Syndrome, also known as MRKH, is a congenital disorder (meaning – born with) which affects 1/5000 women and can be associated with kidney, skeletal and hearing disorders. MRKH is not hereditary or genetic, it is a birth defect that occurs during fetal development and only occurs in females. There is no known cause and there is nothing a mother did or can do to prevent this from happening to their unborn daughter.
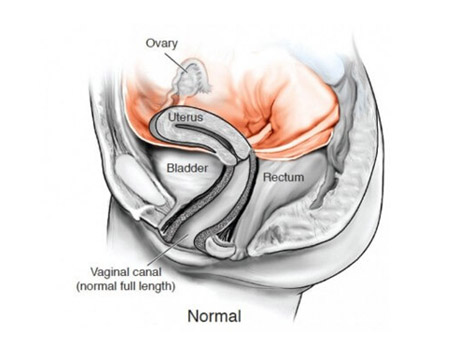
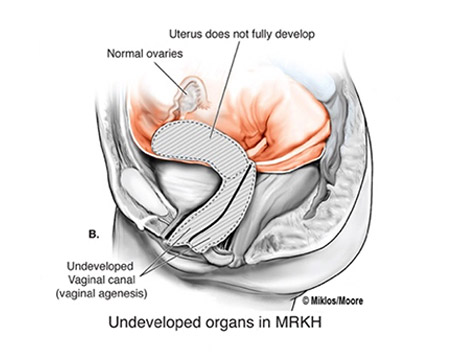
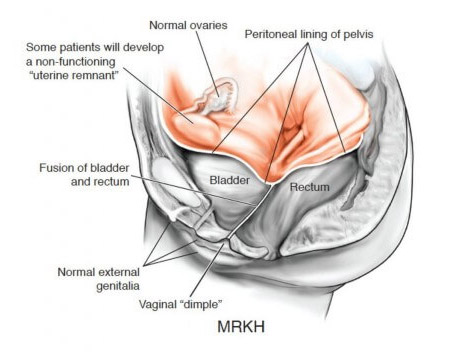
The disease is also known as vaginal agenesis or mullerian agenesis. Most commonly, for unknown reasons, it affects the development of the reproductive tract, specifically, the cervix, uterus and vaginal canal but women with MRKH usually have functional ovaries which are often not seen by radiologist on MRI, CT scans or ultrasound. MRKH causes the vagina and the uterus to be underdeveloped or absent, conditions also known as uterine agenesis and vaginal agenesis. If these conditions are present the young woman will not be able to have menstrual periods and this is what often prompts her to see a physician, thus, most women are diagnosed with MRKH between the ages of 14-18 years. Our other websites: mrkh-surgeons.com and mrkh.com.

Case Study
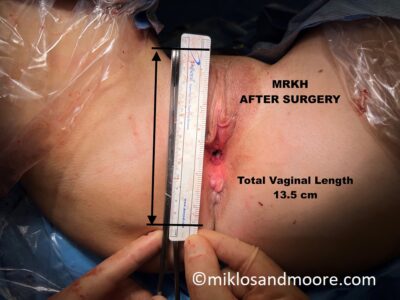
This MRKH patient is from Mexico City Mexico and returned to see Dr Miklos & Moore for a routine check up 14 weeks after her original vaginal lengthening surgery. During her office exam it was noted that she had some raw bleeding tissue which needed to be revised. She was taken to the operating room for the 5 minute surgical procedure and during this small procedure we note the difference between the original vaginal skin and the lengthened skin. It is well documented that the Davydov Neovagina will actually become vaginal skin as it matures. This patient started with a 2.5 cm vagina and her current length is 12 cm.
An MRKH patient is a genetic female with normal female chromosomes (46XX) and normal ovaries and, therefore, develops normal external female characteristics, including breasts and normal appearing external vulva and vagina. She has the physical appearance of a woman because she is a woman!! Examination and studies typically reveal the lack of a vaginal canal or a very short one that would not tolerate intercourse. The diagnosis is one that is very difficult for many young women emotionally to handle, however, the good news is that there are treatment options to allow MRKH patients to achieve full vaginal length and a normal sexual life. Women with MRKH are usually unable to carry a pregnancy, they may be able to have children through other reproductive technologies. There is much hope for the future for patients with MRKH desiring pregnancy as medical, scientific and surgical technology advancements are produced at a lightening pace in the 21st century. Most women who are recently diagnosed with MRKH at a young age address their primary concern, sexual function, first. Drs. Miklos & Moore offer the least invasive and the most effective surgical procedure known for the creation of a vagina, aka, Neovagina. Both doctors have been performing the laparoscopic Davydov Neovagina since 1999 and have had greater than 97% success rate.