Vaginal mesh problems/complications became a common entity after the introduction of the TVT sling into the USA in 1998. Subsequently other surgeries including TOT slings (2002) and single incision slings (2006) as well as other transvaginal mesh procedures for cystocele, rectocele and vault prolapse (early 2000s). Other mesh procedures which are done through the abdomen like the sacralcolpopexy (1970) can also cause problems but have higher cure rates and lower complications than transvaginal mesh surgeries.
Some Vaginal Mesh Surgical Procedures
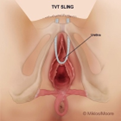
TVT SLING
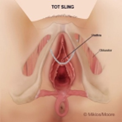
TOT SLING
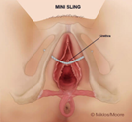
SINGLE INCISION SLING

SACRALCOLPOPEXY MESH
- What are Vaginal Mesh Problems or Complications?
There are many problems or complications that may occur with vaginal mesh Including but not limited to: mesh extrusion, exposure and erosion, infection, incomplete bladder emptying, painful defecation, frequency, urgency of urination, painful urination and intercourse, also known as dyspareunia, and pelvic, abdominal, groin (inguinal), buttocks, and inner thigh pain.
Though these are the most commonly described and scientifically documented complications, it has been our experience that patients can have others Including: fibromyalgia, chronic fatigue, general body aches and pains, recurrent UTI’s (bladder infections), recurrent vaginal infections, pruritis (itching) and other symptoms much like an allergy. No doctor or scientist knows definitively all the potential complications a woman might experience from mesh insertion. No doctor can guarantee removing the mesh will take away any or all of the patients’ symptoms. The only way one will know is to remove the mesh
- Can Vaginal Mesh Problems be Treated without Surgery”
Without surgery, vaginal mesh problems cannot normally or always be fully treated. The type, duration, and symptoms associated with a mesh complication helps the patient and the experienced mesh surgeon determine the correct approach to symptoms resolution. Patients experiencing:
Mesh exposure– is defined as area of mesh without skin coverage which appears to be flat and not protruding above the level of the skin i.e., simply there is no vaginal skin over the mesh. Mesh exposure can be asymptomatic or create pain with or without intercourse and can often be treated with transvaginal estrogen. Often over time the vaginal skin will grow over and cover the mesh. If the skin does not cover over the mesh in approximately 12 weeks the exposed mesh may need to be surgically revised.
Mesh extrusion – is defined as exposed mesh that protrude or sticks out beyond the plane of the vaginal skin. Extrusion associated symptoms may include pain, painful intercourse (aka dyspareunia) to the patient and or her partner, a pinching or pricking sensation in the vagina and a course roughness to the to touch. Estrogen alone will not allow the skin to grow over the mesh as the mesh is protruding beyond the level of the skin. The best solution is to excise the mesh in this immediate area. Obviously if the mesh is protruding a few millimeters one can remove a minimal amount of mesh but if the mesh is extruding 2 – 3 cm (2.54 cm = 1 inch) then a much larger portion of the mesh needs to be removed. If the patient is experiencing pain all the time and not just with intercourse, then the whole mesh implant may need to be removed.
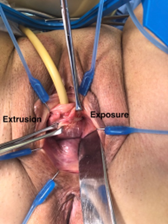
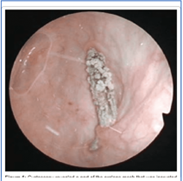
Mesh Extrusion and Exposure
Mesh extrusion on the left side of the photo and mesh exposure on the right side.
Mesh erosion – is defined as mesh which has displaced into a neighboring organ such as the urethra, rectum, bladder or intestines. The most common site of erosion are the bladder and urethra but can also be found in the rectum and the intestines. These patients can experience chronic or intermittent pain as well as pain with urination or defecation. Patients may also experience blood in the urine or feces. Some patients can have recurrent bladder infections if the mesh is in the urethra or bladder. Still other patients do not have any symptoms whatsoever. These patients are usually best managed surgically with complete mesh removal and repair of the damaged organ.
Mesh Erosion
Mesh erosion in the bladder
Mesh infection – is defined as persistent pus drainage or an abscess (pocket of pus) located in direct contact with the mesh implant. These patients usually present with vaginal, pelvic, rectal, buttocks or lower abdominal pain and are found to have an abscess and even a fever. Sometimes the infection can be treated with just antibiotics and others may requires antibiotics and surgery for mesh removal.
Incomplete bladder emptying/Urine retention – is often defined as the inability to expel at least 80% of the bladders content. Often doctors will have a post urination bladder residual as a cut off like 100 mL. In other words, if the patient voids but leaves more than 100 mL in the bladder after the urination (i.e., her urine residual) she is said to have incomplete bladder emptying.
This complication occurs in approximately 1-2 % of the time after a sling, such as TVT, TOT and single incision slings (SIS) which has been placed for stress urine incontinence (SUI). Incomplete bladder emptying or urine retention can occur from placing the sling too tightly or if the mesh slings scars too tightly. This can create an obstructive effect at the urethra inhibiting the emptying of the bladder.
Let me be clear, most patients without a sling, cannot “completely empty” their bladders as most person has some urine residual, but it is the amount of residual which matters (see above). The surgeon determines whether the patient is in retention or has incomplete bladder emptying based upon his/her patient’s symptoms and the amount of retrained urine after urination. If the patient has been diagnosed with retention or incomplete bladder emptying the sling can be cut, partially removed or completely removed based upon the patient’s associated symptoms and clinical picture.
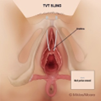
If the patient has obstruction with a TVT sling, then the patient would have a vaginal incision to do a TVT revision or partial removal of the sling. If the retention is associated with lower abdominal, pelvic or suprapubic pain the experienced surgeon will most likely need perform a total TVT sling removal through a large abdominal incision or in more experienced hands through small abdominal incision (i.e., laparoscopically).
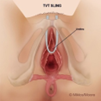
TVT normal
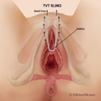
TVT retention
TVT revision

TVT total removal
If the patient has obstruction after a TOT sling, then the patient would have a vaginal incision to remove the vaginal portion of the sling. If the retention is associated with the upper inner thigh, groin, vaginal or pelvic pain the experienced surgeon will most likely need to remove the TOT arms of the mesh through bilateral groin incisions. Very few surgeons in the world have the skill, expertise or experience in removing the complete TOT sling.
Urgency, frequency of urination – is defined by urinating more than 8-10 times per day. Usually there is a significant increase in the frequency of urination after any type of sling procedure when compared to her pre surgical state. The increased in frequency and urgency is often due to a partial obstructive effect of the mesh sling which causes the bladder to spasms. Most often these symptoms will resolve on their own in a couple of weeks or they can be treated with anti-bladder spasm medications and bladder retraining. If the patient’s symptoms do not resolve with medication and bladder retraining and the patient elects, then sling can be removed, and this should, but not always, diminish bladder spasms
Pain – due to mesh implantation usually need to be addressed through surgery. Of course, all patients have some pain after surgery, but normal post-surgical pain resolves with time. If the patient has severe pain immediately after surgery or if the pain persists more than 6 weeks after surgery the patient will probably require complete mesh removal. Of course, each patient must be evaluated independently, and the evaluation and recommendations really depend upon the experience, understanding and expertise of the implanting surgeon.
Most surgeons do not have a basic understanding of mesh complications, treatment or surgical removal as they have not been taught about mesh complications. Though these surgeons may be ignorant mesh copmlciations and treatment they should not be held accountable for their lack of knowledge. Not all surgeons have been trained equally and in my opinion most training programs do not adequately teach the appropriate treatment of mesh complications So, if a patient feels her pain is out of proportion to her surgery especially 6 weeks after surgery the patient should seek an experienced surgeon as soon as possible for evaluation and potential removal of the mesh implant.
- Will Vaginal Mesh Complications Get Worse Over Time”
Over time, vaginal mesh complications generally get worse with few exceptions. Mesh complications usually get worse over time due to the persistent inflammatory reaction the mesh incites from the body. Inflammation is one of the four stages of healing that results in scar tissue formation, proliferation causing contraction and collagen remodeling.
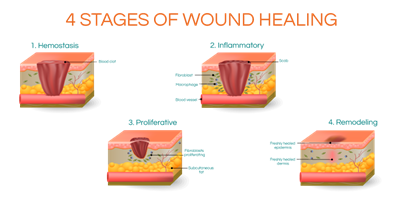
FOUR STAGES OF WOUND HEALING
Scar formation is important and a necessary step of all healing however the mesh enhances and prolongs the 4-step healing process. This occurs due to the constant and chronic irritation and inflammation produced by the foreign body know as mesh. The incision and the mesh trigger the healing cascade of hemostasis, inflammation, proliferation and remodeling and this results in scar. Overtime the scar bridges over the mesh and intertwines in the mesh pores and tightens the mesh making it shorter. This results in a tug of war at the points of mesh attachment pulling on muscles and its associated nerves resulting in a slow persistent increase of pain over time. The longer the mesh remains in place the greater the chance of chronic inflammation, scar maturation and possible chronic, worsening or new onset pain.
Dr Miklos & Moore have personally seen patients who were pain free for upwards of 10 years and then began to have late onsent pain and subsequently needed the mesh removed. Again, this late onset pain is due to the chronic healing process caused by the mesh.
Mesh exposure – if mesh the mesh does not cover over with skin (aka. Re-epithelization) with the use of transvaginal estrogen cream within 12 weeks usually the patient will require surgery to correct the problem
Mesh extrusion – though most surgeons will recommend estrogen cream for the extrusion, this is rarely going to fix the problem because the mesh is protruding above the level of the vaginal skin. The skin will not grow over top of the mesh because of its protrusion which is different than simple exposure. If after 6 weeks of estrogen therapy the vaginal skin does not cover the mesh the patient would best benefits from surgical revision of the mesh and its associated vaginal scar.
Mesh erosion – or mesh found inside the bladder, urethra, rectum or bowel will never get better with time. In fact, most patients go undiagnosed because the surgeon rarely checks for this complication. If a patient suffers from painful urination or defecation, or blood in the urine or feces, the patient should be evaluated for mesh erosion. If erosion is found the only treatment is surgical removal of the mesh and repair of the invaded organ i.e., bowel, rectum, bladder or urethra.
Incomplete bladder emptying – if after approximately 2-3 weeks the patient still has elevated levels of urine left over in her bladder after urinating, most likely this condition will not improve or resolve with time. The patient will need to have a revision surgery of the mesh. Usually this can be accomplished by removing the vaginal portion of the mesh sling underneath and adjacent to the urethra.
Pain– persistent vaginal, pelvic, groin, lower abdominal or pubic pain after mesh implant surgery will usually get worse with time. This complication is usually the worst and most devastating complications of mesh surgery. If the patient’s post-operative pain persists beyond 6 weeks, it has been my experience that this pain will never go away unless the mesh is surgically removed.
Most surgeons will recommend physical therapy or corticosteroid injections to improve the pain. These treatments are considered conservative and you can certainly try them but if there is not an improvement in 6 weeks of therapy if is my experience the pain is NOT going away. In fact, the pain will continue to get worse over time. Though corticosteroids and physical therapy are certainly conservative treatments they are not always the best or most successful therapies. Doctors often chose these therapies because they lack experience in the treatment of persistent pain after mesh implantation.
Example: If one accidentally gets a grain of sand (or mesh) in their eye, is it appropriate treatment to treat the eye with corticosteroid therapy eye drops or massage the eye with the grain of sand in place? The answer is a profound NO!!! In fact, massage of the eye with the foreign body will often result in worse damage or pain to the patient. Most women undergoing physical therapy for vaginal pain will attest to the fact the pain is made worse for several days after the treatment.
The first step in treatment of a foreign body in one’s eye is to remove the foreign body (a constant irritant), then treat with corticosteroids and a gentle massage of the eye to distribute the steroids in the eye fluid. Why would you treat the rest of the human body any differently? Conservative therapy is often prescribed as the average health care professional lacks the appropriate tools to make the diagnosis of mesh complication nor do they understand the appropriate therapies.
- What are The Early and Late Symptoms of Vaginal Mesh Problems?
As referenced above the early symptoms of vaginal mesh problems can include…..frequency and urgency of urination, pain after surgery and possibly difficulty emptying the bladder. Each of these symptoms can be a normal part of the healing process and will usually resolve within a few weeks after surgery. However, they can be considered problematic if they persist (approximately after 6 weeks).
There is no immediate cut off as to what is normal and abnormal. But of the symptoms mentioned above they usually will resolve within 6 weeks after the surgery. If these symptoms persist or new mesh complications presents the patient might consider getting a second opinion from a more experienced surgeon.
As mentioned above mesh continues to interact with the human body and can make symptoms worse over time. Some patients have a gradual increase of symptoms and still others have a delayed response where they don’t present with mesh exposure, extrusion erosion, incomplete bladder emptying, frequency, urgency, painful urination or defecation until months oir years later. Just be aware of that symptoms can occur any time after the implantation and a skilled physician is necessary to make the correct diagnosis.
- How to Choose a Vaginal Mesh Complication Surgeon?
Choosing the best vaginal mesh complication surgeon involves…finding a surgeon who has experience, expertise, credentials and a great reputation. Though no surgeon is perfect, undoubtedly like any profession there are some doctors and surgeons are better than others. It never ceases to amaze Dr. Miklos & Moore that patients will spend more time and money researching a vacation, a new car, a wedding or bat mitzvah than they will on their surgeon. Most often patients will only go to a surgeon that is listed on their insurance plan or at a major university. This is not choosing the best surgeon.
When choosing a surgeon or physician, choose a surgeon or a physician and not a university or an available doctor from your insurance plan. In other words, just don’t say: “I am going to University of XXXX or XXXX Clinic for my treatment because they are the best” because you don’t know what doctor you will be seeing at this institution. You as a patient must research and seek the best surgeon that meets your requirements by reviewing and vetting the surgeon. Check the surgeon for:
- Experience – how many cases have they done
- Expertise – do they do research or write papers or teach lectures on the topic
- Credential – are they appropriately trained and certified
- Reputation – online reviews and even more importantly find another doctor who might recommend a surgeon
- Surgical skill – find an operating room nurse, anesthesiologist, surgical company sales representative from the hospital where he/she operates, these healthcare professionals have usually seen a ton of surgeons and they know who the best are in that hospital.
Dr Miklos & Moore have written many mesh removal papers, some of which are the largest papers on mesh removal in the world. (see above)
Dr Miklos & Moore have had patients with persistent symptoms which were ignored by physicians from some of the most prestigious University or Clinic in the USA. These physicians are no bad physicians but instead, they are physicians who lack knowledge, experience and expertise in the field of mesh complications and treatment.
Drs Miklos and Moore are often asked, “how is it you have more experience than these surgeons or institutions? “ The fact is they were some of the first surgeons in the USA to implant both the TVT sling, TOT sling, mini sling and transvaginal mesh in the USA and have some of the largest mesh surgical papers in the world as well they continue to learn by listening to patients who come to them with complaints. Over time and through the internet they have become a center of excellence for mesh complications and surgical mesh removal.
A perfect example of their experience can be seen in their peer-reviewed scientific paper below:
Indications and Complications Associated with the Removal of 506 Pieces of Vaginal Mesh
Used in Pelvic Floor Reconstruction: A Multicenter Study.
This study, on vaginal mesh complications and problems, was written by Drs Miklos & Moore along with surgeons from Emory University and Cleveland Clinic. In this scientific study, 506 pieces of vaginal mesh were removed from patients in 3-year time period. Dr. Miklos & Moore surgically removed 80% (400/506) of the mesh compared to 12% by Emory University and 8% by the Cleveland Clinic. This constitutes skill, experience and expertise.
So, vet your surgeon wisely. Don’t assume that going to a private surgeon is better than going to a university or world established clinic. Nor assume that going to a well-established renowned clinic is better than a community surgeon. Do your research and choose a surgeon only after spending the time to figure out his/her qualifications and remember: “your body and your health is the most important investment in your life” treat it accordingly.






