WHAT ARE THE SIGNS AND SYMPTOMS OF A FAILED TVT MESH SLING?
The TVT mesh sling is made to treat stress urine incontinence i.e., SUI. If one places a TVT sling and it doesn’t correct the SUI, then that would be considered a failure. The patient would feel leakage with coughing and sneezing and the healthcare professional could see the leakage during an exam.
A failed TVT slings might also mean the leakage has been corrected, but the patient is having other problems that affect her quality of life. The most common complications associated with a TVT sling are as follows:
Chronic Pain – is one of the most common & most devastating complications of transvaginal mesh surgery. This can be caused by nerve damage, mesh erosion into neighboring organs such as bladder, urethra, rectum, small or large bowel or most commonly the vaginal skin or excessive scar tissue which can pull on nerves resulting in pain.
Painful sex – the mesh can cause painful intercourse for the patient and/or her partner. Again, the scar tissue can cause pain by tension on nerves or exposure, extrusion, or erosion of mesh.
Infection – is caused by an overgrowth of bacteria which is creating an inflammatory reaction of the bladder and/or vaginal wall. The infection can manifest as symptoms of pain, fever or discharge.
Mesh exposure – is defined as mesh seen through a defect in the vaginal skin, however, this mesh does not protrude above or beyond the level of the skin. Mesh exposure can cause bleeding, infection, pain or painful intercourse for the patient and/or her partners.
Mesh extrusion – mesh is exposed through the skin but is protruding above or beyond the borders of the skin.
Mesh erosion – is like mesh exposure however instead of the mesh migrating or being seen on the outside i.e., as a disruption in the skin of the vagina one would see the mesh penetrating the inside of a neighboring organ such as the urethra, bladder, or rectum. When this happens common signs or symptoms include pain, bleeding, infection, painful intercourse or potentially blood in the urine or in the feces and pain during urination or defecation.
Urinary problems – may include urinary retention, incomplete bladder emptying, urgency, frequency, night time urination, overactive bladder, recurrent urinary tract infections or UTI’s or urinary incontinence.
If you are experiencing any of these signs or symptoms after undergoing mesh surgery, it is important to consult with an experienced mesh removal surgeon or healthcare provider for proper evaluation and treatment. All too often patients are having mesh failures inappropriately evaluated or even treated. Failure to remove the mesh appropriately can lead to further complications and worsening conditions as well as making the remainder of the mesh even more difficult to find and remove in future surgery.
WHY CHOOSE MIKLOS & MOORE UROGYNECOLOGY TO END YOUR FAILED TVT SLING?
Dr. Miklos is a highly experienced and skilled surgeon who specializes in the treatment of mesh complications. He has removed more than 1,000 pieces of mesh and has been removing mesh since 1998. Few surgeons in the world can make this claim. Dr. Miklos has a patient-centered approach to care and listens to the patient’s point of view which is not always supported by the scientific literature. He takes the time to thoroughly evaluate each patient’s unique situation and develop a personalized treatment plan and makes recommendations but allows each patient to make the final decision as to the surgery and technique. He truly believes that he makes the patient an informed consumer so she can make ultimately make the right decision to minimize or stop the patients’ pain and suffering. Overall, choosing Dr. Miklos for your mesh complication surgery can provide you with the expert care and support you need to achieve the best possible outcome. Dr Miklos has:
EXPERIENCE -First and foremost, at Miklos & Moore Urogynecology, the doctors listen. They have been removing mesh since 1998 and have seen, treated, or removed just about every type of transvaginal mesh complication known to man. They have removed more than 1000 pieces of mesh with minimal complications and superior success. The largest USA paper written on mesh removal is a series of 506 pieces of mesh in 3.5 years and Dr Miklos was responsible for removing 400 of the 506 pieces of mesh. (Figure 1) Of the 506 pieces of mesh removed 286 were slings making this paper the largest USA paper on sling removal. Dr Miklos removed the majority of these slings and was the only surgery to remove the total TVT or TOT sling. (Figure 2)
EXPERTISE – Miklos & Moore Urogynecology have treated patients from all over the world with mesh complications. They have produced award winning videos which have gotten them international acclaim for their mesh removing technique.
KNOWLEDGE – Drs. Miklos & Moore are Rule 26 medical legal experts who understand the law and malpractice cases facing patients today. They are also leaders in the world on mesh complications as they have written some of the largest papers on mesh complications found in the worldwide literature.
RESULTS – Miklos & Moore Urogynecology have addressed and removed some of the most difficult transvaginal mesh devices made and inserted in the human body. Though no one can guarantee the success rate for fixing the patients symptoms, Dr. Miklos can usually remove >95% of the mesh load > 90% of the time. He can totally remove the complete implant most of the time if the patient so desires or if it is medically indicated.
Here at Miklos & Moore Urogynecology we have removed mesh from inside the urethra, bladder, rectum and small bowel. We have repaired fistulas due to the mesh in the bladder, urethra, and the rectum. We have removed as many as 3 mesh slings in one patient and 4 mesh devices in another patient during one operation. In selected cases, Dr Miklos can also offer reconstructive surgery to repair further prolapse or incontinence after the mesh removal.
RECOVERY TIME AFTER FAILED TVT SLING REMOVAL SURGERY?
The recovery time after failed TVT sling removal surgery depends upon the actual surgical procedure performed as described above. We can essentially categorize the recovery based upon 3 different types of TVT sling removal. (See Medical Illustrations below)
- Transvaginal mesh sling incision or transvaginal mesh sling partial removal. These patients only have one incision under the urethra of approximately 2 cm. After the mesh is either cut of removed, a suture is used to close this 2 cm incision. Usually, the TVT mesh sling is cut or partially removed for urine retention or painful intercourse. This procedure can usually be performed with little postoperative pain and as an outpatient. The patients can usually return to work the next day but are restricted from intercourse for 4 weeks and most patients are pain free in 1-2 days.
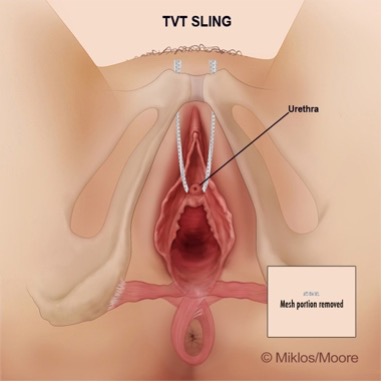
Figure 3
Remove < 2 cm TVT sling
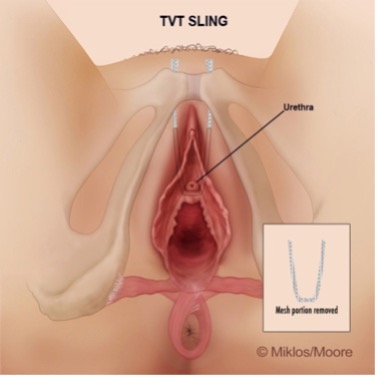
Figure 4
Remove 4-6 cm TVT sling
- Total TVT removal – requires a transvaginal sling removal via the vagina then a laparoscopic TVT arm removal performed through her abdomen. With total TVT removal the patients usually spend one night in the hospital and can go back to full normal activity in 6 weeks. If the patient happens to get a concurrent anti leakage operation like a laparoscopic (non-mesh) Burch or another sling, then the patient is restricted from heavy lifting or intercourse for 6-12 weeks. Most patients are pain free in 1-2 weeks.
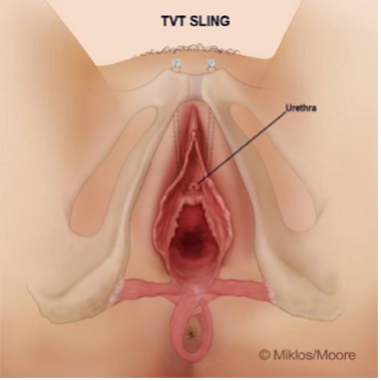
Fig. 5
Remove Total TVT sling
Video 1
Total TVT removal for Pelvic Pain
- Total TVT removal from the urethra, bladder, or bowel. These patients also spend one night in the hospital and can go home the next day. We recommend 6 weeks of pelvic rest, meaning, no sex, heavy lifting or straining until the abdominal incisions heal. If the patient also received a non-mesh anti-leakage operation at the time of the mesh sling removal, she will need to extent her recovery time to approximately 12 weeks. Most patients are actually pain-free within two weeks of their surgery.
Video 2
TVT removal from urethra